Sleep apnea affects millions in the U.S., with several risk factors ranging from obesity to smoking. While the genetic link to central sleep apnea is relatively uncommon, it is more frequently found in obstructive sleep apnea. In fact, research estimates that genetics could be responsible for as many as 75% of these cases.
This article will examine the types of sleep apnea, explore the role of genetics, and explain what a sleep apnea diagnosis involves.
Understanding Sleep Apnea
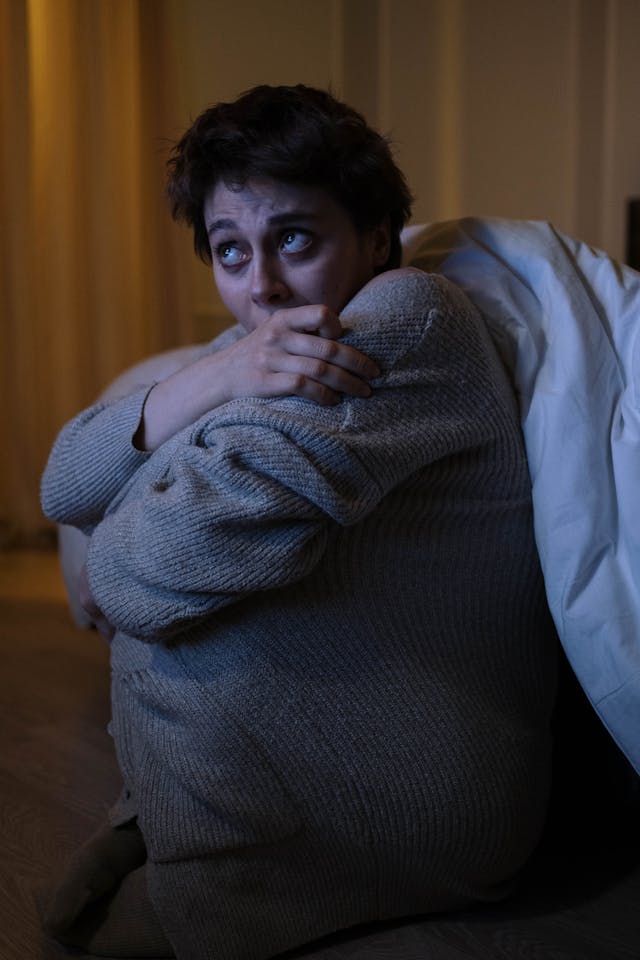
Sleep apnea is a chronic condition characterized by pauses in breathing during sleep. In severe cases of sleep apnea, these interruptions can happen dozens of times in a single night.
Recognizing sleep apnea symptoms is particularly crucial for individuals with a family history of Obstructive Sleep Apnea (OSA), as early detection allows for timely treatment. These symptoms include noticeable loud snoring, choking, or gasping for air during sleep. Daytime sleepiness despite having a full night’s sleep, frequent nocturnal awakenings, morning headaches, dry mouth upon waking, irritability, and difficulties with concentration or memory are also common indications of this disorder.
Types of Sleep Apnea
There are two types of sleep apnea:
- Central sleep apnea occurs when the brain fails to transmit signals to the body to breathe
- Obstructive sleep apnea results when there’s difficulty moving air in and out of the lungs due to an obstruction. This typically happens when the muscles of the tongue and throat relax excessively during sleep, blocking the airway.
Factors Contributing to Sleep Apnea
The causes of sleep apnea vary depending on its type and the age at which it develops.
Obstructive sleep apnea
-
Obesity
A 10% increase in body weight elevates a person’s likelihood of developing moderate to severe OSA sixfold.
-
Body Type
How and where a person stores fat can influence their OSA risk. People with a larger neck or abdomen are at an elevated risk.
-
Facial Anatomy
A person’s facial structure and the positioning of specific bones in the head and jaw can lead to a narrower airway and a heightened risk of OSA.
-
Gender
Men are prone to OSA in young and middle adulthood. However, post-menopausal women have an equal chance of developing OSA. Men and women with comparable body mass index often find that men tend to exhibit more severe symptoms.
-
Age
OSA prevalence increases with age. For instance, research indicates that 10% of men aged between 30 and 40 have OSA, whereas 30% of men above 80 have the condition. This heightened risk may be attributed to reduced time in deep sleep, a natural occurrence with aging.
-
Race and Ethnicity
Studies show that individuals of Black, Hispanic, Chinese, and American Indian descent have a marginally higher OSA risk.
Central Sleep Apnea
Despite the similarity to OSA in terms of the breathing pauses during sleep, the factors contributing to CSA differ:
-
Congestive Heart Failure
Undergoing heart failure typically triggers physiological shifts that heighten the likelihood of CSA. These include increased sensitivity in carotid artery receptors, elevated lung blood vessel pressure, increased sensitivity to blood carbon dioxide level changes, and prolonged blood circulation times.
-
High Altitudes
Even healthy individuals without any CSA history face increased risk when they travel to altitudes of 3,000 meters or more above sea level. Those particularly sensitive might encounter symptoms at lower altitudes..
-
Opioid Use
More than half of chronic opioid users display CSA symptoms during sleep, with the severity corresponding to the opioid dosage. This can likely be attributed to the impact of opioids on the central nervous system.
What Role Does Genetics Play in Sleep Apnea?
Scientists have discovered genetic elements that increase a person’s propensity for developing OSA. On the other hand, CSA, which involves breathing lapses because of issues with brainstem signaling, seems predominantly induced by non-genetic elements.
Research indicates that the risk of developing OSA increases for individuals with close family members suffering from the disorder. Experts estimate that genetics account for approximately 40% of differences in the number of times people experience breathing interruptions (Apnea Hypopnea Index or AHI) during sleep.
Scientists theorize multiple genetic influences could predispose a person to OSA:
-
Body Fat Quantity and Distribution
Genes influence body weight and fat distribution, impacting the likelihood of developing OSA. Obesity increases the risk of having OSA more than tenfold.
-
Facial Structure
Genes significantly affect a person’s facial and skull structure, including skull and nose width, length, and depth. The size and shape of the nose and the positioning of the jaw and other bones can affect the width of the airway and its susceptibility to blockages.
-
Breathing Regulation
Though research on genes and breath control is sparse, experts conjecture genetics could influence the muscles and neural signals involved in breathing, which may affect sleep apnea propensity.
-
Sleep and Circadian Rhythm
A person’s genes affect their innate sleep schedule and sleep quality and whether they have other sleep disorders. Future research is needed to examine how genetics affect sleep patterns concerning OSA.
While researchers have studied sleep apnea genetics for over two decades, specific genes associated with sleep-disordered breathing remain largely unknown. More research is required, but presently, evidence suggests the following genes might be related to intermittent hypoxia or involved in OSA:
- Angiopoietin-2 gene (ANGPT2)
- Lysophosphatidic acid receptor 1 (LPAR1)
- −308G/A polymorphism of the tumor necrosis factor-α (TNFα)
- Serotonin receptor encoding gene (HTR2A)
- G-protein receptor gene (GPR83)
- Dopamine receptor D1 encoding gene (DRD1)
- β-arrestin 1 gene (ARRB1)
- Prostaglandin E2 receptor EP3 subtype (PTGER3)
Though more research is needed, genetic elements contributing to OSA could partially explain why the disorder affects various races differently. Genetics could also clarify why OSA is connected to many other conditions. The related research is still in the early phases, but genes linked to both OSA and high triglyceride levels have been identified.
Sleep Apnea Solutions in Oregon
Obtaining a restful night’s sleep is crucial to your overall mental and physical well-being. And yes, while OSA has a genetic component, an effective treatment option is available. At Sleep Metrics, we offer comprehensive sleep studies and provide CPAP therapy supplies.
To find out more, contact us today!